What is Critical Care Medicine?
Critical Care Medicine is the multiprofessional healthcare specialty that cares for patients with acute, life-threatening illness or injury. It’s a unique specialty in how it encompasses support of multiple organs that might be failing, making it a backbone of any healthcare institution and a cornerstone for its success. Patients was taken of in units synonymously names Intensive Care Unit (ICU), Intensive Therapy Unit (ITU) or Critical Care Unit (CCU). We might all experience critical illness, not only as patients, but as family members or friends of those who are critically ill. Furthermore, Critical Care Medicine extend beyond the confounds of a physical space, to a scene of an accident, in emergency medical services, and in the operating rooms or wards, while these early minutes and hours of critical interventions make a big difference in patient outcomes.

Critical care is provided by interprofessional teams of highly experienced and professional physicians, critical care nurses, respiratory therapists, clinical pharmacists, clinical nutritionists, perfusionists, speech and language pathologist and other allied health professionals who use their unique expertise, ability to interpret important therapeutic information, access to highly sophisticated equipment and the services of support personnel to provide care that leads to the best outcome for the patient. While the continuum of critical care begins at the time of illness or injury, it continues throughout the patient's hospitalization, treatment, and subsequent recovery and beyond discharge from the ICU.
How did Critical Care Medicine start?
While Critical Care Medicine as we know it today is considered a very young specialty, there are some historical recognitions of acute and life-threatening illness that required to group patients in specific location is any hospital. From observation beds next to nursing stations, to specialized post-surgical units looking after complex surgical interventions in USA in the early 20th century or during World War II and formation of shock wards.
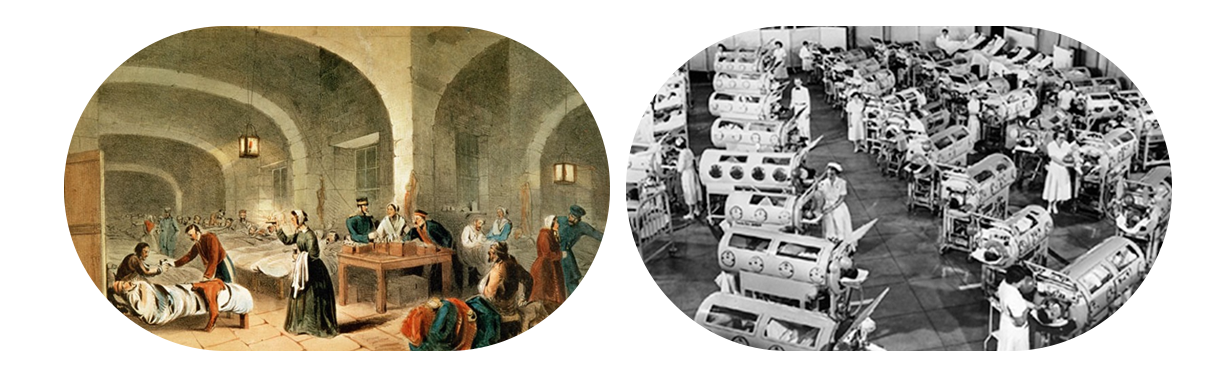
Not until the polio pandemic that hit Europe and the United States in the mid 20th Century, Critical Care Medicine units forms in the way we know it today with the creation of modern positive pressure mechanical ventilation delivered via tracheostomy in Denmark and respiratory paralysis could be supported and improved survival. These new formed units spread in the 1950’s across Europe, United States hospital and then across the world to deliver highly intensive therapies that needed close monitoring of the sickest patient in the hospital.

Throughout the end of the 20th century and early 21st century, Critical Care Medicine developed further to include in its core evidence-based medicine and expansions of its to include complex surgical procedures, multivesical transplantation, advanced therapeutics for respiratory and cardiac failure, complex neurocritical care, advanced management of shock from different etiologies, care for patients with burns and trauma due to different causes and uses on non-invasive modalities of care. Furthermore, effects of Critical Care Therapies on patients and caregivers have been recognized and factored into care and longitudinal follow-up of patient even after discharge from Critical Care.

Who are the members of the Critical Care Team?
The critical care team includes a diverse group of highly trained professionals from different disciplines and areas of expertise and could vary between hospitals. An optimal team would include

Intensivists:
Physicians who are board certified in a medical specialty, such as internal medicine, anesthesiology, surgery or pediatrics, and who also receive special education, training, and subspecialty certification in Critical Care Medicine. Rather than focusing on specific body systems – like cardiologists (the heart and vascular system) or respirologist (the lungs and respiratory system) – intensivists take a comprehensive approach to caring for critically ill patients. The intensivist has the primary responsibility for the ICU patient’s care versus acting as a consultant, as many specialists do. In this role, he or she leads a team of caregivers who are experts in different specialties. The intensivist also oversees the many decisions involved in a critically ill patient’s care, and coordinates all the other services the patient may need – including those from specialists. Intensivists may also coordinate the administrative environment of the ICU by setting policies, developing protocols, and facilitating communication among different specialists, patients, and their families. When intensivists follow the evidence-based guidelines for intensive care, there are well-documented benefits that include:
- Improved patient outcomes, including survival rates
- Reduced complications
- Shorter lengths of stay in the ICU
- Enhanced medication safety
Critical care nurses:
Nurses whom provide a high level of skilled nursing for total patient care and often facilitate communication between all of the people involved in the care of the patient. Their expertise and continuous presence allows early recognition of subtle, but significant, changes in patient conditions, thereby preventing worsening conditions and minimizing complications that arise from critical illness. Because of their close contact with the family and the patient, critical care nurses often serve as the patient's advocate and become integral to the decision-making process of the patient, family, and critical care team.
Respiratory Therapists:
Therapists who work with the critical care team to monitor and promote airway management of the critical care patient. This may include: oxygen therapy, mechanical ventilation (breathing machine) management, aerosol medication therapy, cardio-respiratory monitoring, and patient and caregiver education.
Perfusionists:
a certified medical technician responsible for operating and maintaining equipment’s providing extracorporeal life support in all its forms.
Clinical Pharmacists:
A pharmacist certified in the science and clinical use of medications. The pharmacist with specialty training in the ICU is equipped in recognizing the needs and problems specific to the critical care patient and work with members of the health-care team to foster effective and safe medication therapy.
Clinical Nutritionist:
A dietician is a vital part of the medical team that consults with physicians, nurses, therapists, and family members in the ICU. The dietician works to improve the nutritional health and promotes recovery of the critical care patient.
Physiotherapist Therapists and Occupational Therapists:
The physical therapist provides services that restore function, improve mobility, relieve pain, and prevent or limit permanent physical disabilities. The occupational therapist is trained to make a complete evaluation of the impact of the disease on the activities of the critical care patient at home, in work situations, and recreational activities. Both members work cooperatively with other disciplines of the healthcare team to reduce physical and psychological disability of the patient.
Speech and Language Pathologists:
a specialist who works to prevent, assess and treat speech, language, social communication, cognitive-communication and swallowing disorders in children and adults.
History of Critical Care in Kuwait
Critical care in Kuwait have gone through an evolution that echoed the development of the specialty globally. It started with dedication acute monitored beds starting with Al-Amiri Hospital in 1949, and then subsequently all the major general and subspeciality hospitals that have been established. With establishments of anesthesia as a specialty, these acute monitored beds expanded to allow more advanced and prolonged surgeries to be started and supported. Furthermore, there have been need for further acute beds between cardiology and internal medicine in the early 70’s, therefore these beds and units became the early critical care units and were run in combination between anesthesia and different specialties like internal medicine, cardiology, respirology and surgical specialties. Not until the year 2000, where the first trained intensivist, Dr Kefaya Abdulmalek, joint the Ministry of Health after finishing her training in Canada and established the first closed ICU in 2002 as we know currently. This was followed by different closed units being established with the different intensivists re-joining the Ministry of Health after finishing their training.












